Author
Author: Hiral Patel, MHS, CRC
This two-part blog series will discuss the inclusion of prosthetics in life care plans and the different types of prosthetics. Over 185,000 people in the United States have an amputation each year.[1] The most common causes for amputations are vascular disease, trauma, and cancer.[2] Life care plans usually address future care for amputations due to trauma. Trauma causes 45% of all limb loss.[3] The two main categories of amputations are upper extremity and lower extremity. Part 1 will discuss prosthetics and care for lower extremity amputations. Part 2 will discuss prosthetics and care for upper extremity amputations.
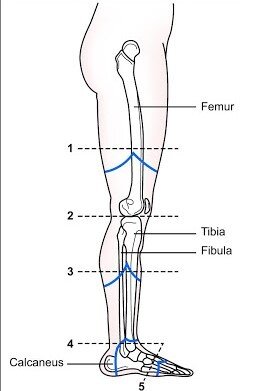
Types of Lower Extremity Amputations
Lower extremity amputations account for 65% of all amputations.[4] Trauma is responsible for only 5.8% of lower-limb amputations.[5] The levels of lower extremity amputations include:
- Above the knee (AKA) (transfemoral)
- Through knee (knee disarticulation)
- Below knee (BKA) (transtibial)
- Ankle (ankle disarticulation- Symes)
- Forefoot (transmetatarsal)[6]
After the amputation, skin closure and infection must be managed. Sometimes a stump revision is necessary for proper healing and prosthetic fit. Sometimes a stump requires a shrinker to mold the stump to the correct size and shape to fit a prosthetic. Proper limb and skin care are essential for health and mobility. Bacterial and fungal infections from sweat can lead to skin irritation, abrasions and skin breakdown could prevent the amputee from using the prosthesis. An amputee should bathe at night as the residual limb tends to swell in hot water or when dangling in the shower. A BKA should never sleep with a pillow under the knee as it can lead to the inability to bend the knee.
Skin care and prosthetic care is necessary to avoid skin breakdown, ulcers, infections and possible reduced sensation in the residual limb. Washing the prosthetic to be sure it is clean for any contact with the skin will prevent the same complications listed above. If the amputee has any problems with the fit or function of the prosthesis, they should immediately contact the prosthetist.
Prosthetic Selection
A prosthesis is an artificial substitute for a missing body part. A lower limb prosthesis refers to a prosthesis that replaces any part of the lower limb to restore the functional and/or cosmetic appearance of the lower limb or both. This may include artificial components that replace the hip, thigh, knee, ankle and foot. The main purpose of a prosthetic is to allow an individual to function at his or her highest level. The most common prosthetics are for AKA and BKA and those are the focus of this blog.
A physician must first determine if a prosthetic is “medically necessary.” “Medical necessity” means that the physician can prove that the service ordered is the appropriate service for the patient. A prosthetic candidate must have a healed amputation site or stump. When the stump is healed, a physician will often refer the patient to a prosthetist. A prosthetist is a specially trained and licensed clinician who evaluates the amputee, determines the appropriate prosthetic, fits the prosthetic, and trains the amputee to use and maintain the prosthetic. One of the first steps in determining the appropriate prosthetic is to determine what level of ambulator the amputee is or will be. This requires determining the K Level.
What is a K-Level?
A K-Level is a rating of amputee’s ability to ambulate based on the Medicare Functional Classification Level,.[7] The rating is from 0 through 4 and indicates a person’s potential to use a prosthetic device, if a device worked well for him or her, and if he or she completed training to use the prosthetic properly.[8] The chart below defines each level:[9]
| K-Level | Definition |
| 0 | Does not have the ability or potential to ambulate or transfer safely with or without assistance and a prosthesis does not enhance their quality of life or mobility. |
| 1 | Has the ability or potential to use a prosthesis for transfers or ambulation on level surfaces at fixed cadence, typical of the limited and unlimited household ambulator. |
| 2 | Has the ability or potential for ambulation with the ability to transverse low level environmental barriers such as curbs, stairs or uneven surfaces. This level is typical of the limited community ambulator. |
| 3 | Has the ability or potential for ambulation with variable cadence, typical of the community ambulator who has the ability to transverse most environmental barriers and may have vocational, therapeutic, or exercise activity that demands prosthetic utilization beyond simple locomotion. |
| 4 | Has the ability or potential for prosthetic ambulation that exceeds the basic ambulation skills, exhibiting high impact, stress or energy levels typical of the prosthetic demands of the child, active adult, or athlete. |
The prosthetist completes the initial evaluation with input from the patient and uses the definitions above to determine the appropriate K-Level which is used to determine the appropriate prosthetic.
Above the Knee vs. Below the Knee Prosthetics
The level of amputation determines which components of the lower extremity prosthesis will need to be prescribed. The most common lower extremity amputations are below the knee and above the knee.
Below the Knee (BK) – Transtibial
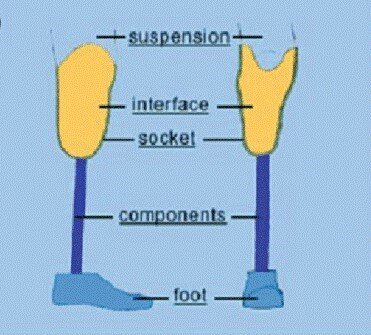
A BKA prosthetic requires a suspension system to keep the prosthetic in place. The prosthetist will determine which system is best. There are three types of suspension systems:
- A vacuum suspension creates a seal around the top of the socket and then a pump removes the air between the socket and the liner as it is worn.
- A shuttle lock is a liner used on the stump with a pin at the end inserted into a “shuttle” lock built into the bottom of the socket.
- A suction system is a soft line with a one-way valve and sealing sleeve. This system adheres the entire interior section of the socket for security and stability.
Above the knee (AK)- Transfemoral
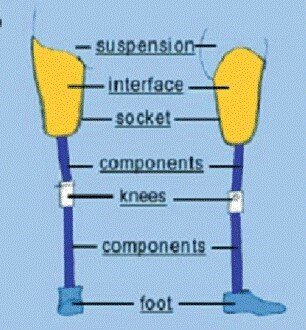
The main difference between a below the knee and an above the knee prosthesis is the AKA requires a knee joint. Functionality depends on selecting the correct knee to fit the person’s age, health, activity level, and lifestyle. Without the knee joint, an amputee would likely have problems with balance and stability and require increased energy to ambulate. The latest or most advanced knee joint is not the best choice for every amputee. For some, safety and stability are the most important consideration. Others who are more active may prefer a knee joint that delivers a higher level of function even if it is more difficult to control.
Types of Prosthetic Knee Joints
Single-axis knee Joints are built with a single hinge point. This type of knee joint is both durable and lightweight, but offers a limited range of adaptability to different gait speeds. Most single-axis knee joints include the ability to lock the knee joint in place for standing or walking when the user needs more security in his prosthesis.
Multi-axis/Polycentric knee Joints bend through multiple hinge points, making it less likely that the knee joint will buckle during standing. In some designs, this mechanism also shortens the prosthesis as it swings beneath the user, reducing the risk of tripping and falling. Polycentric knee joints meet the needs of people for different activities, with simpler versions better for light activity and more advanced versions better suited to heavy activity.
Hydraulic and pneumatic knee joints use air or fluid to adapt to different walking speeds as the wearer swings the leg forward and backward. Some designs allow the user to lock the knee for stability while standing for long periods of time, or when walking in unfamiliar or unsafe environments. Hydraulic and pneumatic knee joints are best for moderately active people who want to vary their walking speeds.
Computerized/Microprocessor knee joints use technology that offers safer walking with less effort, making it easier to navigate hills, ramps, and uneven terrain with greater stability. Microprocessor knee joints are best for people with moderate to active lifestyles who navigate uneven terrain or more basic environmental obstacles like curbs and sloped surfaces. They are especially good for bilateral amputees, as microprocessor knee joints help users feel safer and more confident in daily activities.
Types of Prosthetic Feet
As when selecting a prosthetic leg, several factors must be considered to select the best foot. These include the amputation level, age, weight, foot size, activity level, and occupational needs. Prosthetic feet can be connected to the prosthetic shank with a rigid connection (articulated) or a hinged ankle mechanism (non-articulated).
Solid Ankle Cushioned Heel (SACH) and Elastic (flexible) Keel Foot The simplest non-articulated foot is rigid and provides stability but little lateral movement. It is available in different heights to match individual shoes.
Single-Axis Foot – The articulated single axis foot has an ankle joint that allows the foot to move up and down, enhancing knee stability. The more quickly the full sole of the foot is in contact with the ground, the more stable the prosthesis becomes. This helps users with an amputation anywhere between the knee and hip. The wearer must actively control the prosthesis to prevent the knee from buckling, and the single-axis ankle/foot reduces the effort required to do so. Unfortunately, the single-axis ankle adds weight to the prosthesis, requires periodic servicing, and is slightly more expensive than the more basic SACH foot. A single-axis foot may be more appropriate for individuals where stability is a concern.
Multi-Axis Foot – Similar to the single-axis foot in terms of weight, durability and cost, the multi-axis foot works better on uneven surfaces. The multi-axis foot can also move from side to side.
Dynamic-Response Foot – This foot is best for people with more active lifestyles who vary walking speed, change directions quickly or walk long distances. Dynamic-response feet store and release energy during the walking cycle by absorbing energy in the keel during the “roll-over” phase and then springing back to provide a subjective sense of push-off for the wearer. These have a more normal range of motion and a more symmetrical gait pattern.
Microprocessor Foot – This foot/ankle mechanism has small computer-controlled sensors and adjusts to various needs. Based on input signals, these processors apply an algorithm, or set of rules, to decide how to position the ankle, how to set the damping resistance in the ankle, and how to drive the ankle motor. This foot can react to varying situations with different r alignments to improve the user’s balance and mobility. The goal of this class of prosthetic feet is to mimic the functions of the human foot.
Life Care Planning for Amputees
Life care planners should include all the prosthetics and supplies an amputee needs. They vary based on age, skin integrity, activities, type of prosthetic, length of time used, and other factors. The life care plan should be individualized to meet the individual’s needs.
The Life Care Planning Life Care Planning and Case Management Handbook, Fourth Edition[10] is used in all life care planning courses. Chapter 12, “Life Care Planning for the Amputee,” states the usual and customary charge for a prosthesis is the full, non-discounted, non-Medicare cost, “Almost never is this price paid to the prosthetist for the final prosthetic device. The more appropriate number to use for prosthetic costs is the Medicare allowable reimbursement.”[11] Medicare uses “L codes” to identify specific prosthetics.[12]
A prosthetic device can last anywhere between two to five years. This depends upon the wear and tear from use, age of the amputee and the actual parts. Some parts are easily repaired which allows longer use of the prosthetic.
Most prosthetic devices have warranties ranging from 24 to 36 months after purchase. The life care planner should not include a maintenance cost for the years the device is under warranty.
There are also prosthetic devices designed specifically for showering or swimming which have waterproof parts. There are also “blades” made from carbon for runners. There are prosthetic with flexion and extension movements specifically designed for downhill skiing and snowboarding and similar prosthetics for wakeboarding. BKA can purchase a foot attachment to fit into their prosthetic which then fits into the binding of snow skis. Special feet are also made for rock climbing and there are foot attachments to allow hockey players or skaters to perform on ice.[13]
Conclusion
Prosthetics are constantly being improved with new technology. In the last ten years, lower limb prosthetics have improved:
- Custom sockets distribute mechanical forces more evenly through the residual limb rather than solely bear weight on the residual stump.
- Polymers make prosthetics lighter and more durable.
- There are also advancements for skeletal attachments of prostheses.
Life care planners need to carefully follow developments in prosthetics so the prosthetics and supplies included in a life care plans best meet the needs of each amputee.
Resources
Centers for Medicare & Medicaid Services Health Technology Assessments. Lower Limb Prosthetic Workgroup Consensus Document. September 2017.
Amputee Coalition Website. Prosthetic Knee Systems. https://www.amputee-coalition.org/resources/prosthetic-knee-systems/
Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. Southern Medical Journal. 2002;95(8):875-879.
Hanger clinic https://hangerclinic.com/prosthetics/lower-limb/prosthetic-knees/
Amputee Coalition Website. A Guide to Activity- Specific Prosthetics for Sports
[1] Owings M, Kozak LJ, National Center for Health S. Ambulatory and Inpatient Procedures in the United States, 1996. Hyattsville, Md.: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 1998.
[2] Amputee Coalition Website. Limb Loss Statistics. https://www.amputee-coalition.org/resources/limb-loss-statistics/
[3] Ziegler‐Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation2008;89(3):422‐9.
[4] Amputee Coalition Website. Limb Loss Statistics. https://www.amputee-coalition.org/resources/limb-loss-statistics/
[5] Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. Southern Medical Journal. 2002;95(8):875-879.
[6] Marcovitch H, editor. Black’s Medical Dictionary. London: A&C Black Publishers, 2005.
[7] Crowe et al. Plast Aesthet Res 2019;6:4 I http://dx.doi.org/10.20517/2347-9264.2018.70
[8] inMotion. Volume 23, Issue 5. September-October 2013.
[9] Centers for Medicare & Medicaid Services Health Technology Assessments. Lower Limb Prosthetic Workgroup Consensus Document. September 2017.
[10] Weed, R. and Berens, D. (2010) Life Care Planning and Case Management Handbook. Fourth Edition. CRC Press.
[11] Weed, R. and Berens, D. (2010) Life Care Planning and Case Management Handbook. Fourth Edition. CRC Press. Page 351.
[12] Weed, R. and Berens, D. (2010) Life Care Planning and Case Management Handbook. Fourth Edition. CRC Press.
[13] Amputee Coalition. Website: https://www.amputee-coalition.org/activity-specific-sports-prosthetics/. Accessed May 27, 2020.

